News
Don’t sleep on two important new changes hitting Jan. 1: Mandatory TEAM model and CMS-HCC V28 full payment shift
By Brian Murphy January 1 is rapidly closing in, and 2026 is bringing new rules and regulations impacting the mid-revenue cycle. Here’s two you shouldn’t forget about. Consider this a public safety announcement. V28 of CMS-HCCs Say goodbye to V24, and hello (fully) to V28. This one feels manageable. We’ve all been dealing…
Read More2026 OPPS final rule does no favors for our nation’s hospitals
By Brian Murphy The OPPS final rule, incredibly late this year, is finally out. Here I piece together some thoughts on (generously) four hours of sleep after a late night trip to Boston to pick up my daughter from a weekend getaway, so excuse any illogic. You can read the fact sheet easily enough (see…
Read MoreTrump administration’s appeal of vacated RADV rule indicates Medicare Advantage audits not going away
By Brian Murphy Nothing is over. We’re still deep in the wild west of Medicare Advantage (MA). In case you missed the breaking news over the Thanksgiving break, the Trump administration on Friday appealed a crucial court decision. In September a TX judge ordered the 2023 Risk Adjustment Data Validation (RADV) rule vacated, removing CMS’…
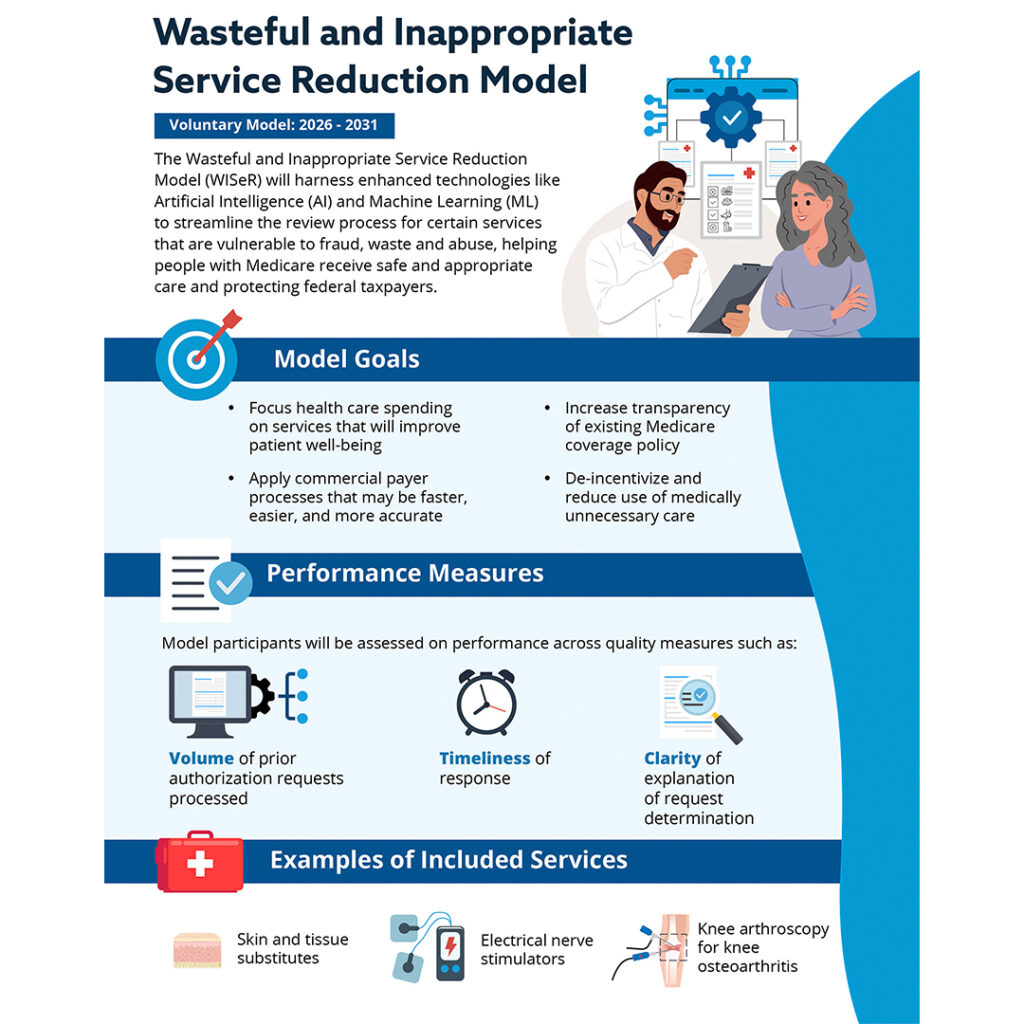
Read MoreNew WISeR model puts CMS squarely in the preauthorization business, for the first time
Effective Jan. 1, 2026, CMS is getting into the prior authorization business. The Wasteful and Inappropriate Service Reduction (WISeR) Model is a pilot program set to run for six years, initially in six states: New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington. It introduces new prior authorization processes for certain high-risk Medicare Part B services…
Read MoreThe State of Provider Engagement
A Norwood special report Download the report here. CDI trends come and go. Retrospective reviews become concurrent and then, prospective. At the elbow record review goes remote. Regulations and code sets change, too: ICD-9 gives way to ICD-10, DRGs to MS-DRGs and HCCs. Today artificial intelligence is the buzzword and the reported cure for all…
Read MoreFrom Risk to Revenue Clarity: How One Health System Transformed OP CDI Performance
Register here: https://my.demio.com/ref/v1rDIDccDyru0SEW Only 31% of U.S. healthcare organizations have a dedicated outpatient CDI program—yet risk-based contracts, MSSP performance pressure, and documentation complexity are accelerating every year. The result? Most organizations are unknowingly leaving substantial RAF revenue unclaimed, exposing themselves to avoidable compliance risk, and missing the chance to influence performance before 2026 benchmarks lock…
Read MoreTelehealth requirements loosened, one of many changes in 2026 MPFS final rule
By Brian Murphy Sizable changes are coming Jan. 1 to telehealth, chronic illness and behavioral health management and reimbursement, and physician payment formulas per the recently released 2026 Medicare physician fee schedule final rule. I’ve summarized a few I find interesting. Telehealth commitment. I’m most excited about these changes. In a long overdue move CMS…
Read MoreBlue Cross Blue Shield of Massachusetts to downcode high level E/M codes for outlier providers
By Brian Murphy We’ve got another blanket E/M downcoding policy set to take place on Monday, just after Halloween. Not a treat. Not a totally unexpected trick, either. A large insurer in my home state of Massachusetts, Blue Cross Blue Shield of MA, will review E/M claims from providers who consistently bill at levels 4…
Read MoreThe power of a pilot: How one organization took flight with OP CDI
Implementing an outpatient CDI program across a large integrated healthcare organization with nearly 80 physician practices and a half-dozen urgent care and community medical centers, all at once, is a daunting task. Too much for one partner organization to bite off. We agreed, and so in June 2024 got them off the runway with a…
Read MoreMedicare Advantage feels like the Wild West — don’t wander off the trail. Download our special report
In May CMS dropped one of the biggest announcements since the advent of ICD-10: An exponential increase of Medicare Advantage (MA) risk adjustment audits. The agency planned to hire 2,000 coders, ramp up its tools with AI and tech, and launch a full-on audit storm. We were all braced for extrapolated, multi-million-dollar recoupments of every…
Read More