Posts by Norwood Staffing
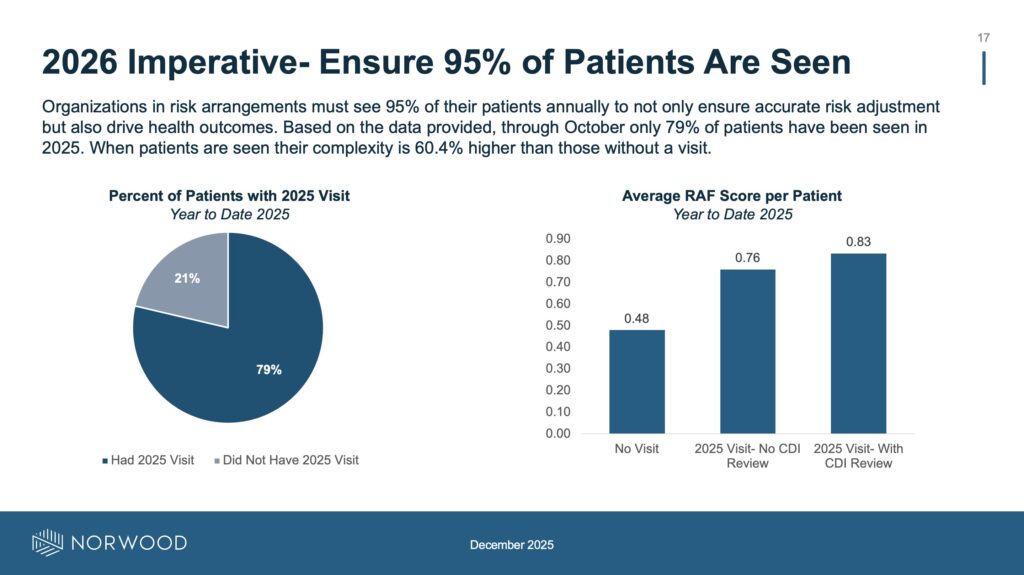
What outpatient CDI transformations are on your 2026 roadmap? Norwood has 45 in its playbook.
By Jason Jobes As 2025 draws to a close, a question: How are you feeling about your value-based care efforts? Are you capturing risk across your organization, effectively and compliantly? Maybe you want to get better. Maybe you just want to get started. If so, here’s a few ideas from a webinar I presented on…
Read MoreOutpatient OG: Amy Campbell on Pre-Visit Reviews, Pet Peeves, and People Management
Listen to the episode here. Outpatient CDI is still in its pioneer-”ish” stage. Why do I say that? Per the most recent ACDIS survey data, only 31% of respondents indicated their organization had a dedicated OP CDI program. Progress, but not enough, and still a minority. So when you find an “OG” who has been…
Read MoreFrom Resistance to Results: Provider engagement from the front lines
Listen to the podcast here. No matter how great your CDI program is—its spectacular workflow, outstanding chart review team, on-point KPIs, shiny new AI tools—nothing works if you don’t have engaged physicians. It still all comes down to provider engagement. Without a physician staff who is bought in and willing to participate and document with…
Read MoreCoaching Clinicians, Convincing Crowds: Susanna Baddiel on Delivering Impactful Presentations
Listen to the podcast here. Fans of Off the Record may recall my recent episode with Chris Petrilli, Director of Revenue Cycle of Operations at NYU Langone, who joined me to discuss his experience delivering a TEDx Talk on artificial intelligence. Chris was well prepared and delivered a great lecture, which you should definitely check…
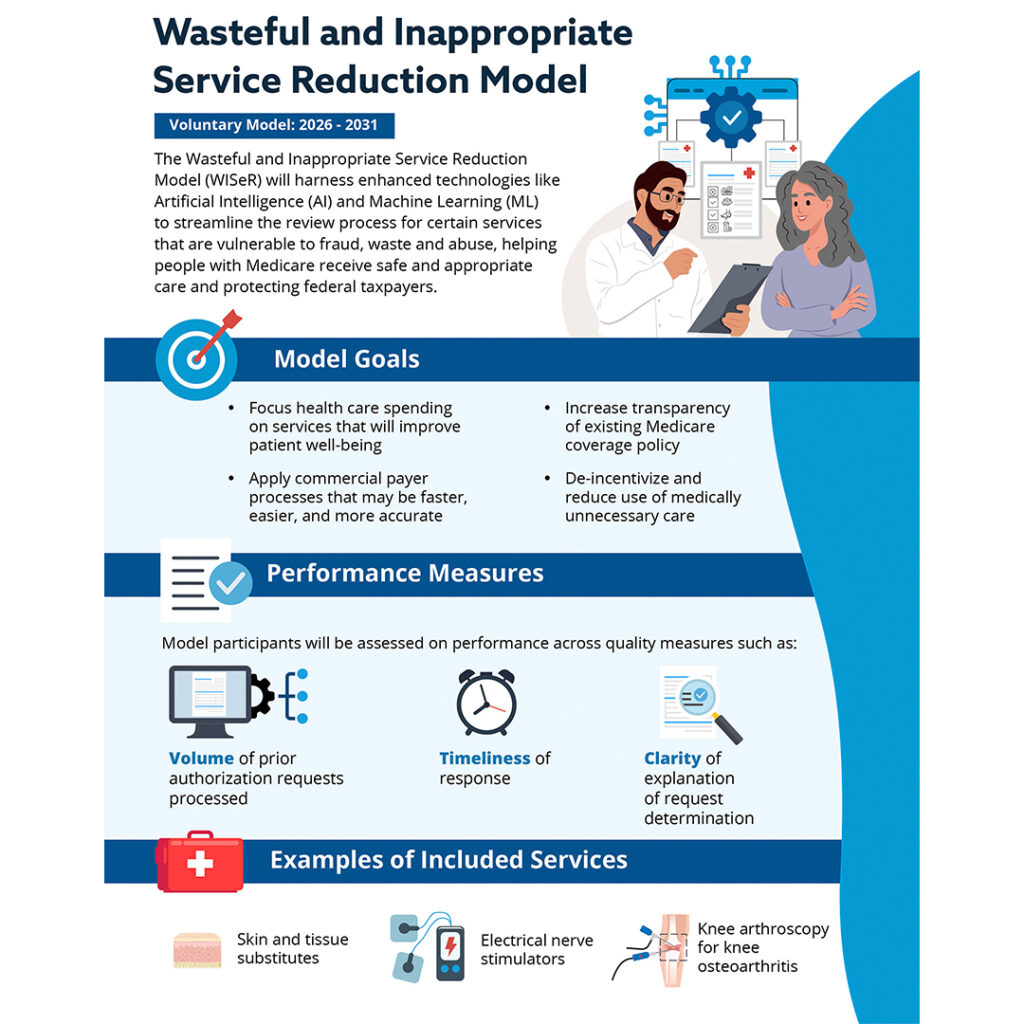
Read MoreNew WISeR model puts CMS squarely in the preauthorization business, for the first time
Effective Jan. 1, 2026, CMS is getting into the prior authorization business. The Wasteful and Inappropriate Service Reduction (WISeR) Model is a pilot program set to run for six years, initially in six states: New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington. It introduces new prior authorization processes for certain high-risk Medicare Part B services…
Read MoreThe State of Provider Engagement
A Norwood special report Download the report here. CDI trends come and go. Retrospective reviews become concurrent and then, prospective. At the elbow record review goes remote. Regulations and code sets change, too: ICD-9 gives way to ICD-10, DRGs to MS-DRGs and HCCs. Today artificial intelligence is the buzzword and the reported cure for all…
Read MoreFrom Risk to Revenue Clarity: How One Health System Transformed OP CDI Performance
Register here: https://my.demio.com/ref/v1rDIDccDyru0SEW Only 31% of U.S. healthcare organizations have a dedicated outpatient CDI program—yet risk-based contracts, MSSP performance pressure, and documentation complexity are accelerating every year. The result? Most organizations are unknowingly leaving substantial RAF revenue unclaimed, exposing themselves to avoidable compliance risk, and missing the chance to influence performance before 2026 benchmarks lock…
Read MoreTelehealth requirements loosened, one of many changes in 2026 MPFS final rule
By Brian Murphy Sizable changes are coming Jan. 1 to telehealth, chronic illness and behavioral health management and reimbursement, and physician payment formulas per the recently released 2026 Medicare physician fee schedule final rule. I’ve summarized a few I find interesting. Telehealth commitment. I’m most excited about these changes. In a long overdue move CMS…
Read MoreDocumentation with a Pulse: Erin Kreider on ethics, CDI advocacy, and ambient listening
Listen to the episode here. Erin Kreider gives me hope for the future of the CDI profession. That’s a pretty positive first impression for someone I recently met. Why do I say this? Erin is a newly-minted clinician who returned to medical school after nursing and CDI to become a nurse practitioner (NP), and now…
Read MoreBlue Cross Blue Shield of Massachusetts to downcode high level E/M codes for outlier providers
By Brian Murphy We’ve got another blanket E/M downcoding policy set to take place on Monday, just after Halloween. Not a treat. Not a totally unexpected trick, either. A large insurer in my home state of Massachusetts, Blue Cross Blue Shield of MA, will review E/M claims from providers who consistently bill at levels 4…
Read More