Posts Tagged ‘cdi’
CDI and Coding Professionals: Indispensable Links in the Chain of Care
By Brian Murphy CDI professionals (and clinically astute coders) can positively impact patient care. How? By being mindful during their chart reviews, noticing documentation discrepancies, and bringing them to the attention of the care team. On the latest episode of Off the Record, Lynne Spryszak, RN, CCDS, gave a couple wonderful examples. Lynne was re-reviewing…
Read MoreCDI, Coding Professionals should Stay Abreast of Proposed HEDIS Measures Changes
Comments to NCQA due March 13 By Brian Murphy The National Committee for Quality Assurance (NCQA) wants your comments on proposed changes to the Healthcare Effectiveness Data and Information Set (HEDIS) measures. That’s a lot of acronyms that you may not think pertain to your job. But HEDIS measures matter. A lot. HEDIS is used…
Read MoreBuilding and Reinventing Pediatric CDI Programs
Thursday, Sept. 21, 1-2 p.m. EST. Register here: https://my.demio.com/ref/Bvi1r8BxSduVGq0b It’s frequently been said (in the context of clinical medicine) that children are not just little adults. You can’t treat them the same way, even with a similar diagnosis. So why should pediatric CDI programs be any different? Pediatric CDI brings with it a unique array…
Read MoreCDI Suggestion: Start your reviews off right with ED/EMS Notes
By Brian Murphy There is no one true way to perform a review of the health record. Some CDI specialists prefer to start with the history and physical before beginning, often 24-48 hours post-admit until significant documentation has been generated. Others want to start immediately after admission with a review of the ED record. Regardless…
Read MoreWill AI Replace CDI Professionals?
In Clinical Documentation Integrity, a primary focus is which technology is the most beneficial – Natural Language Processing (NLP) or a deeper learning Artificial Intelligence (AI). There are different avenues healthcare systems can take when determining how to structure the technology needs for CDI programs. Consider if you want the assistance from information already written…
Read MoreNurse-Led CDI?
Our CDI model at Norwood is Nurse-Led, Physician-Sensitive, Coding-Supported, and Patient-Centered. I’ve been asked about this a few times – as I believe we are the only program that explicitly states “nurse-led”. Most outpatient CDI programs are physician-led. I completely understand and respect this as healthcare has traditionally been led by physicians. Over the last…
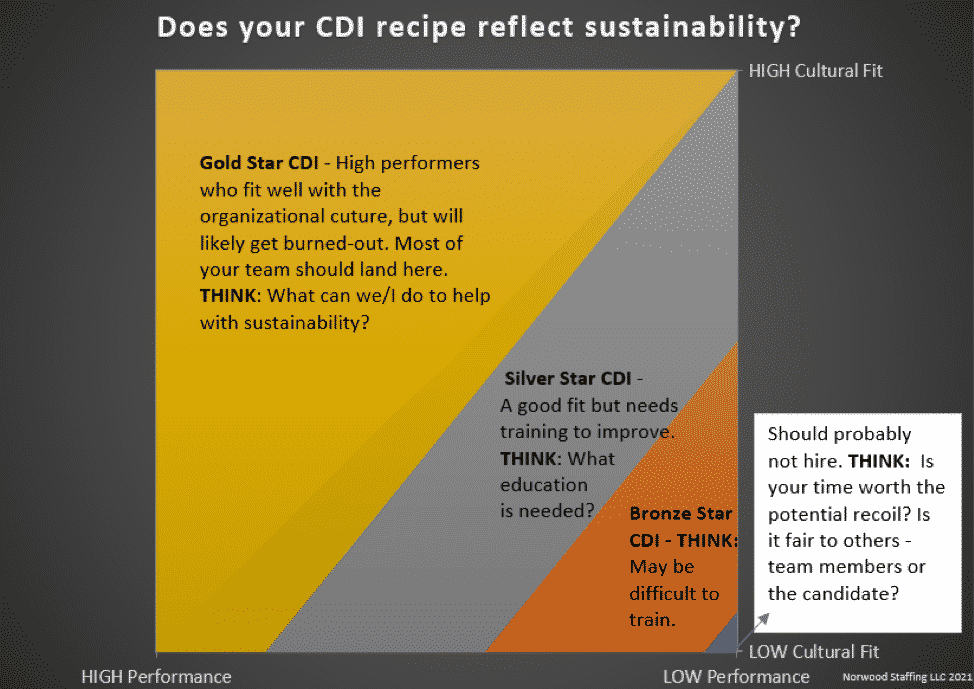
Read MoreGrandma’s Apple Pie.
Who is baking in your CDI kitchen? In the spirit of our theme for CDI week, “CDI Kitchen: Recipes for a Successful Program”, I was thinking about the perfect recipe for a well-functioning CDI program. So many are searching to fine tune the recipe – to get the consistency just right. Unlike a perfectly measured…
Read MoreCan CDI Programs Really Make a Difference?
I have heard it said that the overall goal of Clinical Documentation Integrity (CDI) is to improve documentation for coding and reimbursement. Even though this is in fact a valued outcome of many CDI programs, I argue that it is not the overarching goal of CDI today. With the ensuing complexity of technology, such as…
Read More