CDI, Coding Professionals should Stay Abreast of Proposed HEDIS Measures Changes

Comments to NCQA due March 13
By Brian Murphy
The National Committee for Quality Assurance (NCQA) wants your comments on proposed changes to the Healthcare Effectiveness Data and Information Set (HEDIS) measures.
That’s a lot of acronyms that you may not think pertain to your job. But HEDIS measures matter. A lot.
HEDIS is used by more than 90% of U.S. Health Plans, and accounts for nearly 40% of NCQA accreditation scoring and is factored into Medicare Advantage Plan Star Rating evaluations.
Although HEDIS measures assess the performance of health plans, all the care is of course provided by hospitals and physicians, who contract with these plans. Quality ratings and reimbursement are directly tied to HEDIS measures, and following their recommended courses of treatment a must.
Which means if you’re reading this, they probably impact you and your work.
HEDIS currently includes more than 90 measures across the following six domains of care:
- Effectiveness of Care
- Access/Availability of Care
- Experience of Care
- Utilization and Risk Adjusted Utilization
- Health Plan Descriptive Information
- Measures Reported Using Electronic Clinical Data Systems
But the type and number of changes are constantly changing. The payer Cotiviti published a wonderful article (link below) summing up proposed changes to the HEDIS sets effective for the 2025 Measurement Year (MY). These include five new measures, five revised measures, and additional updates to promote gender and race equity.
To cover all these changes is not possible in a single post, so I’ll refer you to the article below. While you’re there you can sign up for a free webinar series that walks through the year in HEDIS.
Just to look at one proposed change:
Acute Hospitalization Following Outpatient Surgery (HFO)
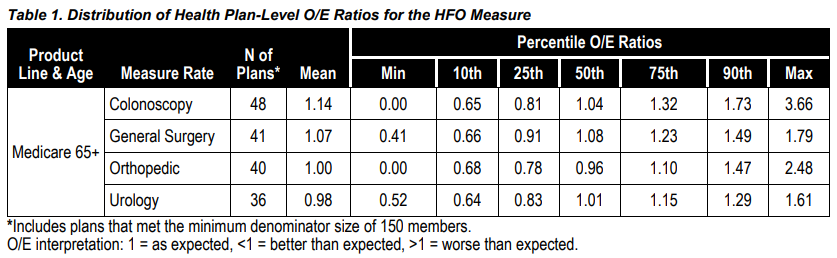
For Medicare Advantage beneficiaries, this risk-adjusted utilization measure would capture the percentage of select outpatient procedures that were followed by an unplanned acute hospitalization for any diagnosis within 15 days, and the predicted probability of an acute hospitalization. This would include four rates:
- Colonoscopy
- General surgery
- Orthopedic procedures
- Urology procedures
This new measure seems to make sense to me (keep I’m mind I’m not a clinician). You probably wouldn’t expect an unplanned acute hospitalization for a colonoscopy patient within 15 days of his/her procedure. If one occurs, that is probably an appropriate “ding” on your performance measure. The accompanying graphic shows the observed/expected (O/E) ratios for each type of surgery.
… unless of course that patient was afflicted with a host of chronic illnesses, with a host of comorbid conditions. The key modifier in the HEDIS measure description is “unplanned.”
A CDI professional or clinically astute coder can help get patients into the right measure through their review work. While I don’t know exactly how these particular measures risk adjust, HCC capture can influence expected readmission rates.
I’m linking to a previous article I wrote on this subject (“Risk adjustment coding and HEDIS measures: Birds of a feather”) below for examples.
The NCQA is accepting public comments on these proposed measures changes through March 13. I’ll write a followup article when the new measures are finalized.
References:
Cotiviti, “NCQA releases proposed HEDIS MY 2025 updates”: https://www.linkedin.com/pulse/ncqa-releases-proposed-hedis-my-2025-updates-cotiviti-7hpue
National Council on Aging, Seven Medicare Advantage Quality Measures You Should Know: https://www.ncoa.org/article/7-medicare-advantage-quality-measures-you-should-know
NCQA, HEDIS and Performance Measurement: https://www.ncqa.org/hedis/
Norwood, “Risk adjustment coding and HEDIS measures: Birds of a feather”: https://www.norwood.com/risk-adjustment-coding-and-hedis-measures-birds-of-a-feather/
U.S. Department of Health and Human Services, “Healthcare Effectiveness Data and Information Set (HEDIS)”: https://health.gov/healthypeople/objectives-and-data/data-sources-and-methods/data-sources/healthcare-effectiveness-data-and-information-set-hedis
Related News & Insights
Code Red: Aligning Risk Adjustment with CMS’s New Audit Mandate
Listen to the episode here. For this week’s episode I’m bringing you something a little different,…
Code Red: CMS announces massive audit expansion of Medicare Advantage, raising risk adjustment coding questions
By Brian Murphy For a while I felt like this was coming to a head. As far…


