Rules and rules: CMS releases burdensome Medicare Advantage final rule with three-year phase-in
By Jason Jobes
CMS has once again shown that it has no concept of the administrative burden it places on providers that ultimately detracts from their ability to provide quality care.
There simply is so much to say about the final CMS Medicare Advantage rule.
Let me start by saying I don’t think anything in the final rule announcement is earth-shattering. Much of the document (+/- 200 pages) is spent replying to comments. I highly recommend that you read the comments around risk adjustment. I will expand on these with my thoughts and additional analysis in the near future.
That said, let’s jump in.
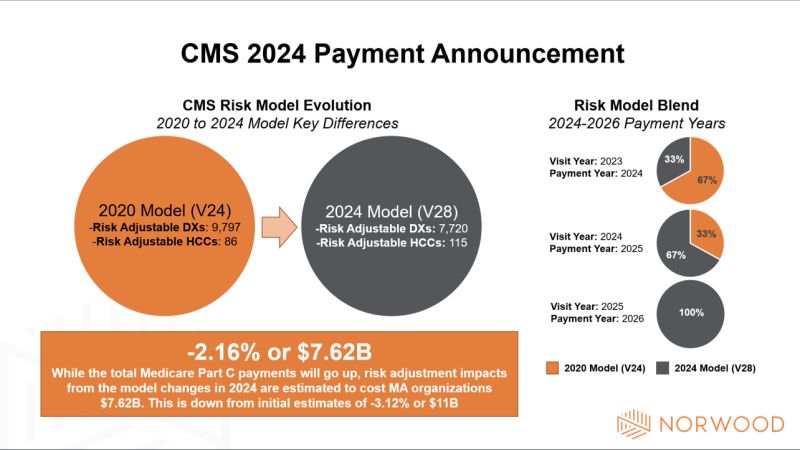
I will start with my biggest problem with the final rule. Electing to phase in the V28 model over three years seems counterintuitive and unproductive. I recognize that many organizations (I heard significantly more noise from payers) expressed concern about the -3.12% impact to risk scores. Let me say that this concern is very warranted, as that was projected to be an $11B impact. Absorbing that shock to the system during a shaky economy could easily produce headwinds that would have a ripple effect. I have no problem with those concerns.
The final rule made adjustments to the effective growth rate and the MA risk score trends that offset much of the model score impact. The phasing in of the model reduces the impact of the risk model revision from -3.12% to -2.16%.
My question is at what cost will shaving 30% of the impact have on provider operations.
Provider organizations often do not have the same resources payer organizations enjoy for managing risk. Their focus is to care for patients while operating a sustainable, profitable business. Many do not employ actuaries, and the ability to obtain claims data, RAF scores, and additional information from their payer partners can be cumbersome. What this means is, provider organizations have to rely on others for information while doing what they can to validate accuracy.
The three-year phased in V28 model puts extreme burden on provider organizations to calculate risk scores, reconcile data with payers and CMS, and live in a hybrid world—all while attempting to move to value-based payment partnerships. Asking organizations, providers, clinical documentation specialists and HCC coding professionals to live in a blended model world shifts additional responsibility and administrative burden to those charged with improving health and access.
Payers: I recognize this isn’t all roses for you either. That said, I would encourage you to use this rule as an opportunity to enhance support to provider partners so that they can help leverage your insights to improve care and outcomes.
Providers: In my opinion the final rule’s impact hurts you the most and as a byproduct your ability to provide care. For those in traditional Medicare value programs (REACH/MSSP) this means you need to sharpen your risk adjustment measurement acumen to ensure you are receiving full credit.
To read additional Norwood analysis of the Medicare Advantage rule, click here: https://www.norwood.com/2024-final-medicare-advantage-rate-announcement-phases-in-v28-changes-icd-10-code-removals/
Related News & Insights
Code Red: Aligning Risk Adjustment with CMS’s New Audit Mandate
Listen to the episode here. For this week’s episode I’m bringing you something a little different,…
Code Red: CMS announces massive audit expansion of Medicare Advantage, raising risk adjustment coding questions
By Brian Murphy For a while I felt like this was coming to a head. As far…


