Posts by Norwood Staffing
Opinion: Put away the CC/MCC strawman, CDI critics
By Brian Murphy It’s time to put away an old, oft-beaten strawman. CDI is way, way past the days of just CC/MCC capture. I still see this myth perpetuated, often in the context of “CDI programs are out of touch and only capture CCs and MCCs. Now buy our product!” I have no doubt…
Read MoreVersion 25 of AHRQ Patient Safety Indicators (PSI): Review these important updates
By Brian Murphy The AHRQ updated the Patient Safety Indicators (PSI). But before we get into them, first a reminder of what PSIs are and why they matter. PSIs provide information on potentially avoidable safety events. Each PSI has inclusion criteria (who/what gets counted; the at-risk population) and exclusion criteria (codes or conditions that…
Read MoreRethinking Rankings: A Smarter Approach to Hospital Quality with Cheryl Manchenton
Listen to the show here Cheryl Manchenton and I go back a long way—I once took a ride from a Las Vegas casino to the airport with her after an ACDIS conference well over a decade ago. And I’ve learned over the years she also happens to be as sharp—and as outspoken—as anyone I’ve ever…
Read MoreNew acute coronary syndromes (ACS) guidelines—what they mean for CDI and coding professionals
By Brian Murphy The American Heart Association/American College of Cardiology in June released updated guidelines on the management of acute coronary syndromes (ACS)—the first time the guidelines have been updated in a decade. I’ve summarized a few nuggets of possible interest for CDI/coding professionals. I always preface these types of updates by saying I’m…
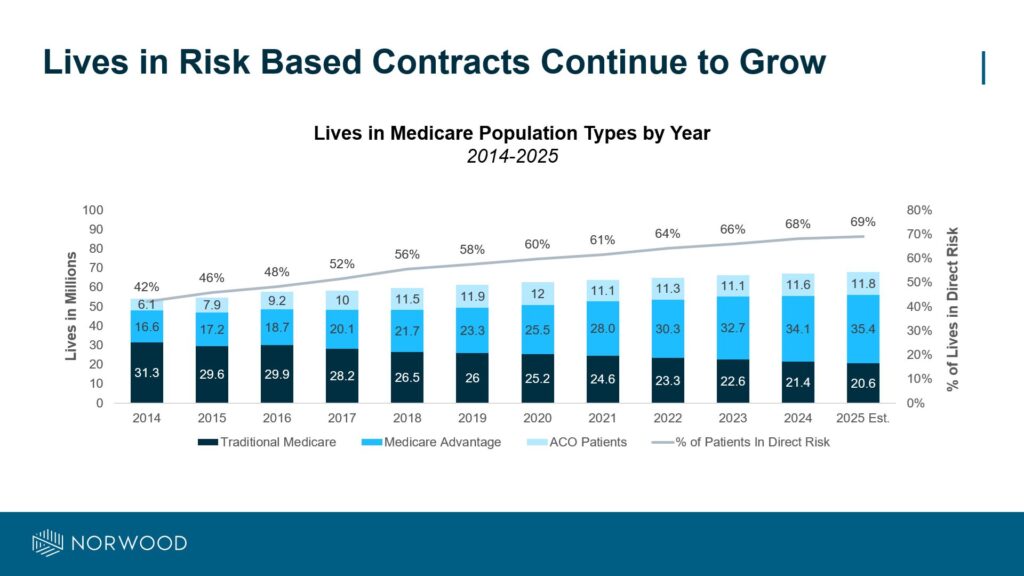
Read MoreWhy Risk Adjustment Accuracy Matters More Than Ever
By Jason Jobes, SVP Solutions Nearly 70% of all Medicare lives are now in contracts that directly tie payment to patient complexity — a number that has surged from 42% in just a decade. As this shift accelerates, organizations must recognize that risk adjustment accuracy isn’t optional — it’s mission-critical. To succeed, leaders need…
Read MoreFrom NYU to TEDx: Chris Petrilli on Tech, Trust, and the Future of Healthcare
Listen to the episode here: https://spotifycreators-web.app.link/e/UQ5dRuNgKVb Some of us dream of being able to say, “Thank you for Coming to my Ted Talk.” Others wilt at the thought of getting on stage to deliver not just a lecture on a complicated or sensitive topic, but a performance. My guest today Dr. Chris Petrilli has delivered.…
Read MoreUnderstanding Medicare Advantage (MA) exploitation of the 3-day stay requirement for skilled nursing facility care
By Brian Murphy The current controversy surrounding Medicare Advantage (MA) plans and the 3-day hospital stay requirement for skilled nursing facility (SNF) care centers on disparities in coverage and potential exploitation of regulatory flexibilities. Let’s break this down. Understanding the 3-Day Rule Under traditional Medicare, beneficiaries must have a medically necessary inpatient hospital stay…
Read MoreCMS TEAM: What it is, how it works … and why I’m an advocate
By Brian Murphy Admission: I’m pro-TEAM. It’s possibly the name but I favor the concept of the new CMS payment model, too. We keep spinning our wheels on the fee-for-service treadmill, which incentivizes volume and often results in unnecessary and fragmented care. Everyone complains about FFS, it’s hard to break free—but TEAM is a compelling…
Read MoreWhat does the RADV Medical Record Reviewer Guidance say about physician queries?
A lot. I’m summarizing it here. See link below, p. 61, for the full monty. Short explanation: CMS conducts annual RADV audits to ensure risk-adjusted payment integrity and accuracy. They use coders to do this; the RADV Medical Record Reviewer Guidance guides their audits. Jan. 2020 is the latest version. RADV auditors are instructed to…
Read More2026 IPPS final rule: TEAM = full steam ahead, Medicare/MA rules consolidation continues, and CC/MCC changes
By Brian Murphy The IPPS 2026 final rule is out… are you ready for some TEAM-work? (ahem) Dad joke aside, the big news IMO is the finalization of a few tweaks to the TEAM model, which is moving full steam ahead for Jan. 1, 2026 implementation. I’ve included a links below for further reading on…
Read More