By Brian Murphy
What actually passed with the new TEAM model—and what does it mean for your organization?
Somewhat lost amid the sea of new regulations and transmittals is CMS’ passage of a new mandatory alternative payment model called the Transforming Episode Accountability Model (TEAM) in the 2025 IPPS final rule.
Per CMS, the intent of TEAM is to improve patient care through holding hospitals financially accountable for certain procedures, called “episode categories.” The hope is that TEAM will reduce Medicare expenditures while preserving or enhancing patient quality of care.
That’s the hope, at least.
Here’s what’s final; keep in mind there are hundreds of pages of regulation so this is a very high-level summary:
- 5-year mandatory model beginning on January 1, 2026, and ending on December 31, 2030. Mandatory means that all seletcted acute care hospitals, with limited exceptions, must participate.*
- Five episode categories, including 1) CABG; 2) Lower extremity joint replacement (LEJR); 3) surgical hip/femur fracture treatment (SHFFT), 4) Spinal fusion; 5) Major bowel procedure. These episodes begin with an anchor hospitalization or procedure and end 30 days after hospital discharge. Specific MS-DRGs and HCPCS billing codes are listed in the rule.
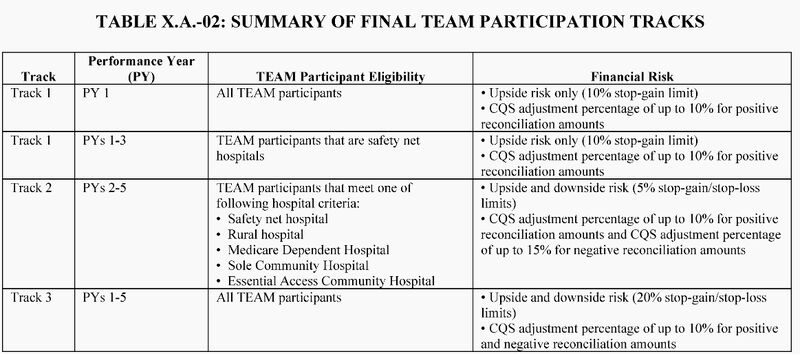
- TEAM participants will continue to bill Medicare FFS as usual but will receive target prices for episodes prior to each performance year. CMS will then compare actual Medicare FFS spending to the target price, as well as by performance on three quality measures. Go below the target price, you get a bonus payment. Above, you will owe CMS a repayment. The amounts are determined by track, year, and hospital type (see graph below).
- The three quality measures in TEAM include 1) Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data, 2) CMS Patient Safety and Adverse Events Composite (CMS PSI 90), 3), Hospital-Level, and Risk-Standardized Patient-Reported Outcomes Following Elective Primary Total Hip and/or Total Knee Arthroplasty (THA/TKA)
- TEAM is risk adjusted for dual eligibility, age, HCC count, and more.
You might (rightly) ask: “It starts Jan. of 2026—why should I care?” Fair point, but, it’s almost 2025 and this is not something you can flip a switch on. And hospitals should be doubling down on performance in the quality measures listed above. Your performance in them will count in TEAM.
I’ll admit it—I’m a fan of this type of program. Care is a fragmented mess right now. Anything that incentivizes better coordination and (hopefully) better patient outcomes is a win in my book, regardless of whether it actually saves money.
TEAM allows providers and suppliers of outpatient therapy services, therapists in a private practice, and therapy group practices to be collaborators in the model. And CMS believes TEAM will spur partnerships between TEAM participants and post-acute care providers, such as skilled nursing facilities and home health agencies, to share financial risk and collaborate on care redesign strategies.
Whether TEAM is the answer remains to be seen. It is extremely complex, and CMS needs to step up with ongoing education over the next year IMO so hospitals can implement it properly.
Implementing it properly and hitting bonuses (and avoiding penalties) will require providers, nurses, CDI, coding, case management, and social workers to work in tandem—plus probably a dedicated TEAM coordinator to make sure milestone sand metrics are being met. This may fall to someone like case management, CDI or HIM, but I believe it will require singular focus.
* Important note: TEAM is mandatory for IPPS hospitals situated within specific geographic regions which they call Core-Based Statistical Areas (CBSAs). CMS has selected 188 CBSAs across nearly all 50 states for mandatory participation. Hospitals located in these designated CBSAs are required to participate in the TEAM model. I recommend reviewing the table in the published in the rule, and contacting CMS’ dedicated email address for questions. See both below.
References
2025 IPPS final rule: https://www.federalregister.gov/documents/2024/08/28/2024-17021/medicare-and-medicaid-programs-and-the-childrens-health-insurance-program-hospital-inpatient
TEAM email address: CMMI_TEAM@cms.hhs.gov.
Related News & Insights
Code Red: Aligning Risk Adjustment with CMS’s New Audit Mandate
Listen to the episode here. For this week’s episode I’m bringing you something a little different,…
Code Red: CMS announces massive audit expansion of Medicare Advantage, raising risk adjustment coding questions
By Brian Murphy For a while I felt like this was coming to a head. As far…


