New WISeR model puts CMS squarely in the preauthorization business, for the first time
Effective Jan. 1, 2026, CMS is getting into the prior authorization business.
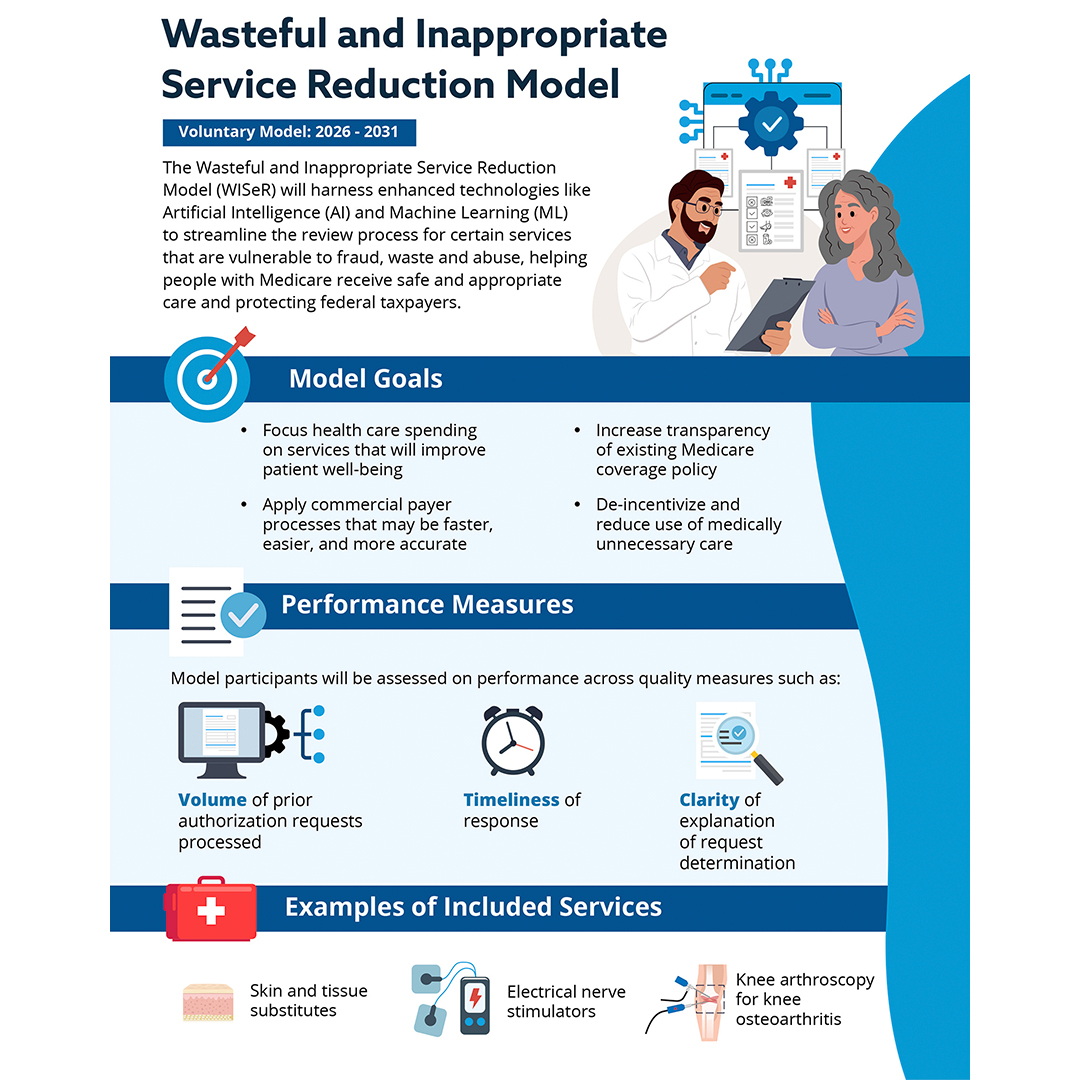
The Wasteful and Inappropriate Service Reduction (WISeR) Model is a pilot program set to run for six years, initially in six states: New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington. It introduces new prior authorization processes for certain high-risk Medicare Part B services to reduce waste, fraud, and abuse.
Here’s what I found most interesting.
The participants in the model are NOT hospitals and providers—though they will be its subjects. Rather, model participants are companies with “expertise providing recommendations on medical necessity of coverage for payers using enhanced technology like AI.”
Model participants will receive a percentage of the savings associated with “averted wasteful, inappropriate care as a result of their reviews,” adjusted based on the participant’s performance on measures related to the process, including provider experience.
Think RAC contractors, except providers who complain overloud could impact their payouts.
Examples of selected items and services in WISeR include:
- skin and tissue substitutes
- implantation of electrical nerve stimulators
- knee arthroscopy for knee osteoarthritis
CMS refers to these as a “subset of items and services that may have little to no clinical benefit for certain patients and that historically have had a higher risk of waste, fraud and abuse.”
CMS plans to use outsourced AI and human clinical review to review claims and potentially deny authorization. All recommendations for non-payment will be determined by appropriately licensed clinicians who will apply standardized, transparent and evidence-based procedures to their review.
The model excludes inpatient-only services, emergency services, services that would “pose a substantial risk to patients if delayed,” and Medicare Advantage patients.
Prior authorization is (mostly) a new concept in Medicare, which traditionally covers services subject to National Coverage Determination (NCD) and leaves medical necessity up to the ordering physician.
There are limited exceptions to this. Some hospital outpatient department services, including certain plastic surgeries, vein procedures, and implantable spinal neurostimulators, are subject to pre-authorization.
But WISeR represents a rather large expansion of government practice of medicine, an odd choice for the current administration and its expressed commitment to removing red tape. But there you have it. CMS believes that some of the above services are being overprescribed and abused—and they may be.
And of course every effort these days seeks to reign in healthcare spending and protect the Medicare Trust Fund.
If you are a provider of the selected items and services above and in one of the impacted six states, I recommend reviewing the model and in particular the Provider and Supplier Operational Guide. It’s a lengthy 61 pages but contains information on specific impacted NCDs and specific documentation requirements.
References
- CMS, WISeR (Wasteful and Inappropriate Service Reduction) Model: https://www.cms.gov/priorities/innovation/innovation-models/wiser
- CMS, Provider and Supplier Operational Guide: https://www.cms.gov/files/document/wiser-provider-supplier-guide.pdf
Related News & Insights
This is what a good outpatient CDI program looks like
By Jason Jobes This, right here. You should be focused on risk score accuracy by simultaneously evaluating how to maximize revenue…
What outpatient CDI transformations are on your 2026 roadmap? Norwood has 45 in its playbook.
By Jason Jobes As 2025 draws to a close, a question: How are you feeling about your…


