Hyponatremia and the bar of query: How much evidence before you clarify the presence of a diagnosis?
By Brian Murphy
How much evidence do you need, or does your organization require, before you send a query?
A broad and difficult question, and obviously much depends on the diagnosis in question. But I’m interested in the big picture.
(As always with these types of posts, I stress that I’m neither a clinician or a coder, just an interested observer).
One of the fascinating elements of CDI work is its relationship to detective work. In fact, it very much reminds me of an old favorite boardgame of mine, Clue. Anyone else play this back in the day? Or perhaps have seen the movie based on the game?
In Clue, players navigate a mansion, moving their pieces from room to room to solve a murder mystery. They need to figure out who committed the crime, with what weapon, and in which room. Players are dealt character, weapon, and location cards, and you work to narrow down the options.
You only get one chance to make an accusation, and if you get it wrong you’re out.
This is a kind of like CDI work. First, you review the medical record (i.e., navigate to each room). Examine the facts of the case. Assemble your evidence. And finally, query the physician (make your accusation).
Like Clue, you won’t have perfect knowledge of the killer (dx), but you’ll have a suspicion, hopefully very strong based on the number of facts (findings).
Some queries will naturally be stronger and more supported than others.
“How much evidence” is becoming increasingly important as payers demand a higher standard for reporting. Per authoritative sources like the ACDIS Pocket Guide, no query should be written without the presence of diagnostic criteria that support the presence of a diagnosis.
One diagnosis that comes up frequently in this context is hyponatremia, ICD-10-CM code E87.1. Per UpToDate, hyponatremia represents a relative excess of water in relation to sodium. It can be induced by a marked increase in water intake and/or by impaired water excretion. Severe cases can lead to cerebral edema and coma. CMS classifies it as a complication/comorbidity (CC) so it has quality and payment ramifications.
Over the years I’ve heard folks say that two low sodium values will trigger a query for the condition. Others want to see the addition of monitoring of these values, which if you know the Official Coding Guidelines, Section III, will satisfy the “other diagnoses” reporting standard:
“For reporting purposes, the definition for “other diagnoses” is interpreted as additional conditions that affect patient care in terms of requiring: clinical validation; or therapeutic treatment; or diagnostic procedures; or extended length of hospital stay; or increased nursing care and/or monitoring.”
To add further complication, monitoring alone may not be enough for some payers, who also want to see treatment.
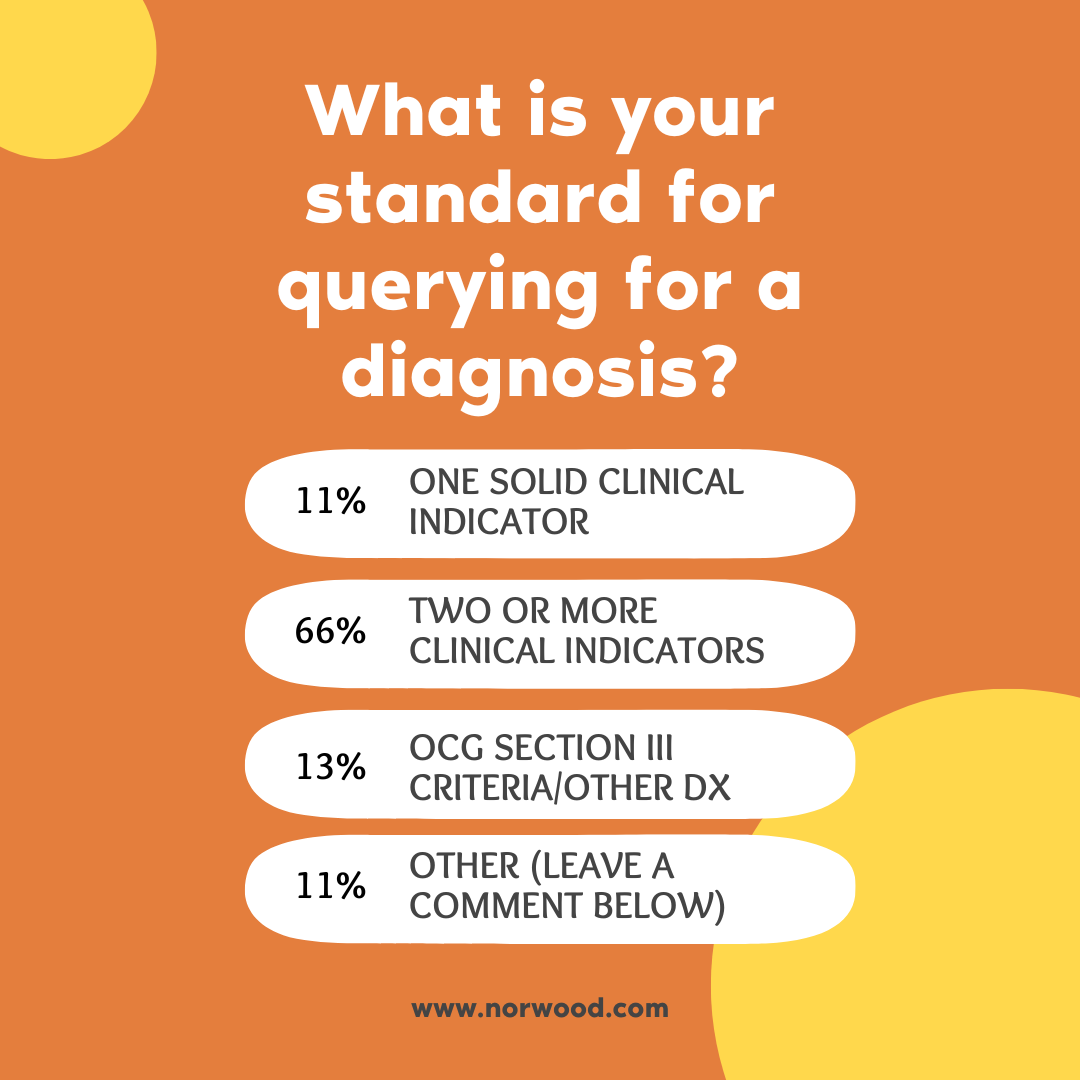
So, when are you ready to accuse (i.e., query), detective, either for hyponatremia, or more broadly? I asked this poll recently on LinkedIn. Here are the results.
What is your standard for querying for a diagnosis?
One solid clinical indicator 11%
Two or more clinical indicators 66%
OCG section III criteria/other diagnoses 13%
Other (please describe) 11%
Of the “other” responses, most said it depends on the diagnosis, with some (including for example sepsis) requiring more than one clinical indicator. Others said a combination of clinical indicator + MEAT criteria.
References
ACDIS, “Q&A: Hyponatremia query for clinical indicators” https://acdis.org/articles/qa-hyponatremia-query-clinical-indicators
CMS, “ICD-10-CM Official Guidelines for Coding and Reporting” https://www.cms.gov/files/document/fy-2023-icd-10-cm-coding-guidelines-updated-01/11/2023.pdf
UpToDate, “Overview of the treatment of hyponatremia in adults”: https://www.uptodate.com/contents/overview-of-the-treatment-of-hyponatremia-in-adults
Related News & Insights
Mid-revenue cycle professionals must ask: What would make our physicians’ lives easier?
By Brian Murphy Every so often—check that, on a regular basis—it pays to step back and think…
Elixhauser: A mouthful to say, but a must know concept in understanding hospital quality and performance
By Brian Murphy Elixhauser. That’s the post. Still with me? I get it. What a name and…


